Reduce audit risk and enhance member experiences
Instead of relying on slow third-party data feeds, incomplete data, and provider frustration, Reveleer delivers accurate, integrated data directly from your provider network.

Accuracy you can count on
Keep your provider directory information current and precise with easy-to-use, industry-leading validation methods.

Fully managed workflow
Free up your team's resources with a continuously validated, comprehensive provider directory data management process.

Maintain compliance and trust
Protect your plan from costly penalties, audit risks, and reputational harm while maintaining trust with providers and members.
How It Works
Automate your provider data collection and accuracy


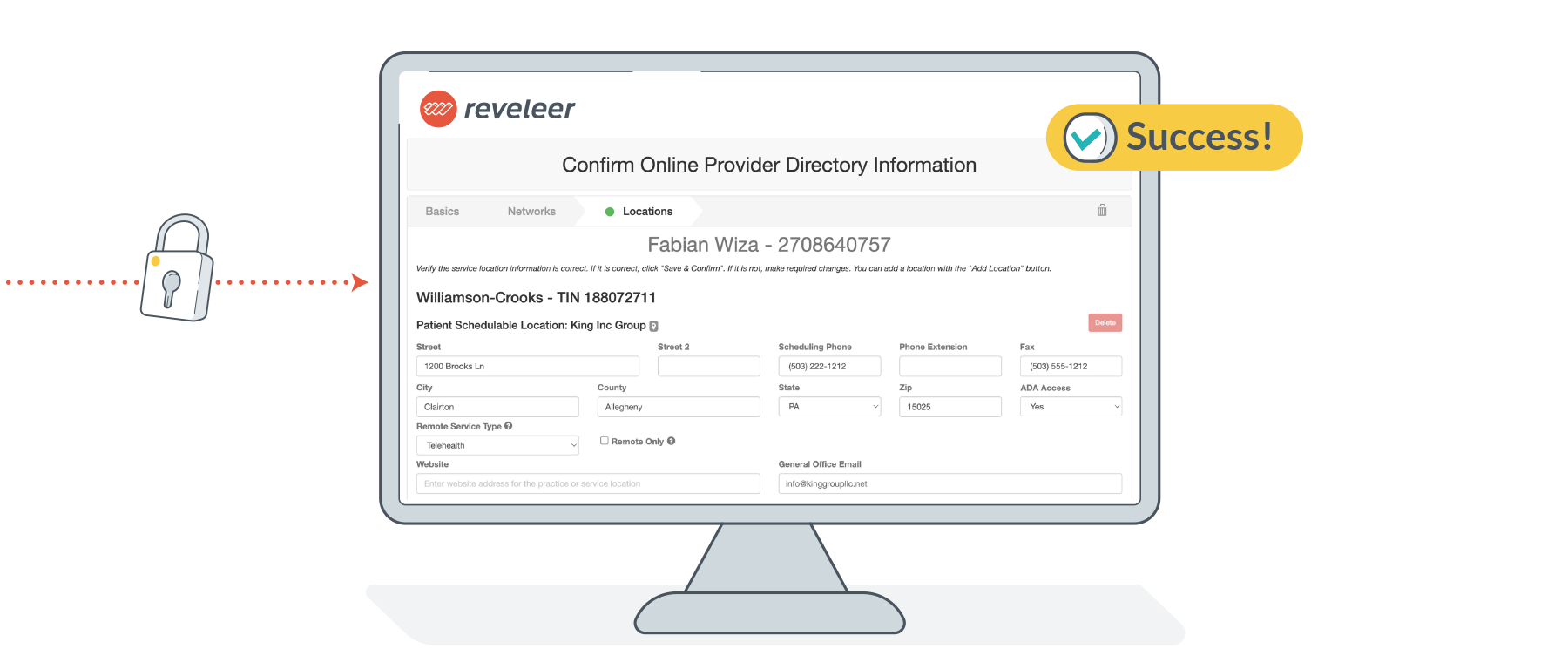
Automate outreach, validate data
Collect accurate provider data directly from the source with automated, user-friendly outreach including email, web forms, and phone. Every record is rigorously validated by advanced data checks and research analysts.

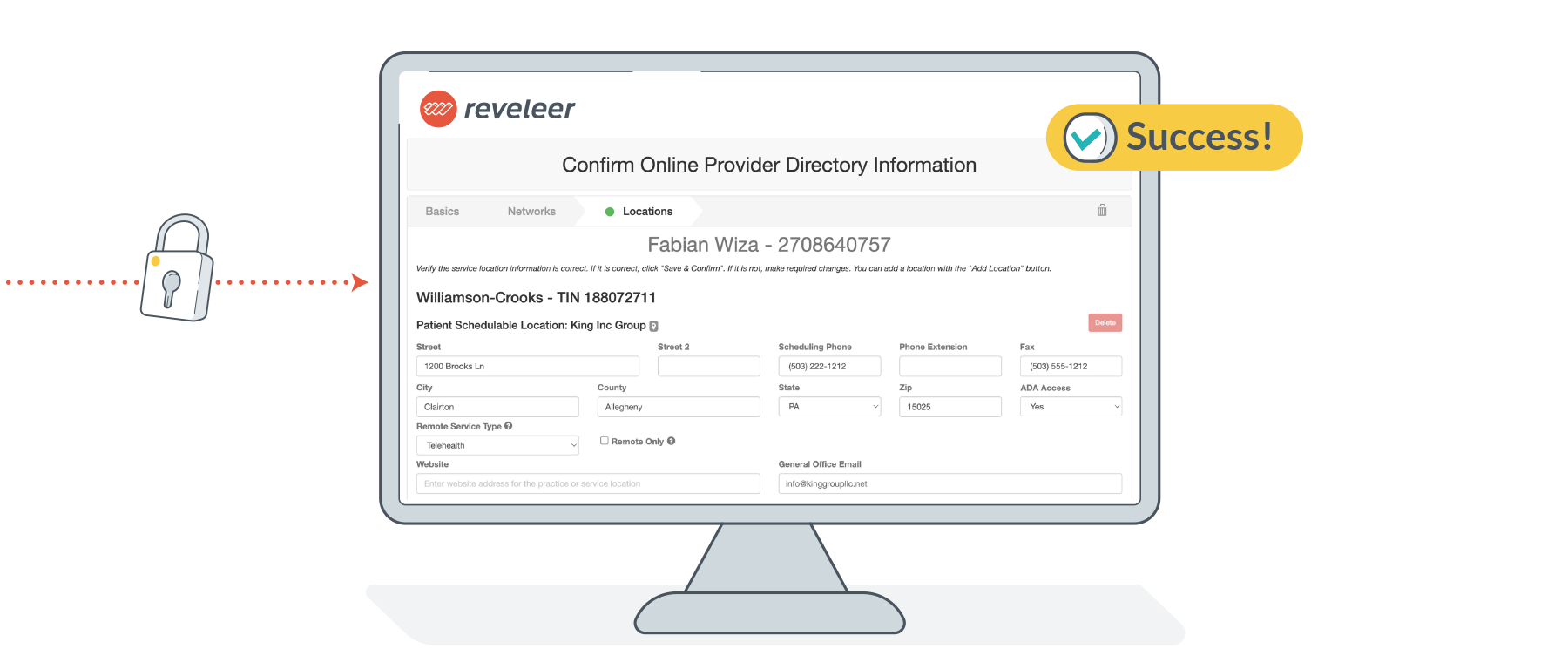
Secure, effortless integration
Reveleer’s secure integrated workflows ensure updated provider data in your existing directories, claims, quality, and network systems. Enable your team members to work from a unified, reliable source.

CMS-compliant data accuracy
Provider data is refreshed quarterly and logged in real time, ensuring ongoing compliance with CMS’s No Surprises Act. Audit trails, dashboards, and instant reporting enables confidence in your provider data throughout the year.

Article
Best practices to fast-track your provider incentive plans
Provider incentive programs can be a powerful tool for health plans to improve quality, close gaps, and motivate network performance. But too often, these programs underdeliver, and providers are left confused and disengaged. In this article we review why today’s incentive programs aren’t working, and what leading health plans are doing differently to motivate their providers.
Key benefits of integrated, easy-to-use provider data validation

Exceptional provider experience
Providers enjoy a simple, fast, and intuitive process for updating their directory data and listings. Over 92% of providers rate the experience as outstanding, ultimately driving valuable relationships, experiences, and satisfaction for your health plan members and providers.
Build trust with your members
Reveleer delivers the most accurate, up-to-date provider directory data that is never scraped or purchased from third parties. Data comes directly from provider sources, collected through a unique outreach process that avoids common provider group abrasion. Maintain CMS-compliance and reduce financial risk with Reveleer.


Unified data across all directories
Flexible provider data management capabilities enable fast, secure updates within EHRs and other connected systems. Most plans achieve CMS compliance within weeks, instead of months which is one of the top reasons customers choose Reveleer’s Provider Profile Validation to collect and validate their provider information.
The essentials of accurate provider directories
How quickly can Provider Profile Validation enable CMS compliance for my health plan?
Most plans achieve full compliance in just a few weeks thanks to our automated outreach, fast integration, and proven workflows.
What is CMS’s No Surprises Act and how can Reveleer help maintain compliance?
The CMS No Surprises Act is a federal law designed to protect patients from receiving unexpected medical bills for emergency services and certain out-of-network care. It also requires health plans to maintain updated provider directories and respond to verification requests from members, with prompt corrections and public access to directory information. Reveleer’s Provider Profile Validation enables CMS-compliance with validating accurate provider data every 90 days. Data updates are logged and easily reportable for audits, CMS, or state regulator requests.
Does Reveleer’s Provider Profile Validation integrate with our existing systems and directories?
Yes, the solution is designed for easy, secure integration with all your provider directories, claims, or quality management systems.
Is the provider outreach process time-consuming or disruptive for our network?
Our managed workflows and automation free up your team's resources to focus on strategic initiatives rather than manual data collection. Providers experience a simple, intuitive update process and consistently rate it very highly. This helps minimize abrasion and increase response rates.
How does Reveleer ensure data accuracy and not just compliance?
We verify updates directly with providers, never scrape or purchase from third parties, and maintain rigorous quality checks with every data refresh.
What results have health plans seen with Reveleer's Provider Profile Validation?
Customers report measurable improvements in accuracy, provider satisfaction (92%+ CSAT), reduced CMS compliance risk, and higher Star ratings.


